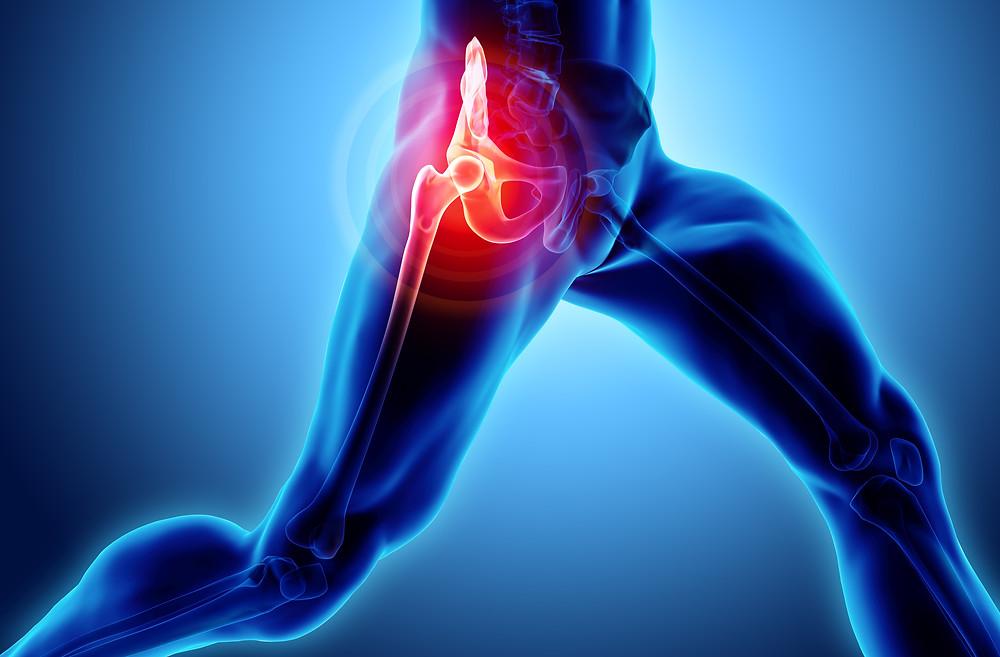
Hip & Knee Replacement; What is Arthritis ?
A smooth, slippery, fibrous connective tissue called articular cartilage acts as a protective cushion between bones inside the joints. Arthritis develops as the cartilage begins to deteriorate or because of wear and tear as part of aging or because of disease like Rheumatoid arthritis. As the articular cartilage is lost, joint space between the bones become narrow. This is an early sign of arthritis and can easily be detected using an X-Rays. Slowly over time the bone ends rub against each other and starts to wear away. This results in progressive pain and shortening. Normal activities like walking and running becomes painful and difficult. Common arthritis symptoms include pain, stiffness, and some loss of joint motion, deformity, limp and shortening of limb
Who develops arthritis?
• Primary osteoarthritis typically affects people over 50 years of age and above, but nowadays it is commonly seen at younger ages also.
• It is more common in persons who are overweight or obese, or suffering from Rheumatoid arthritis or Ankylosing spondylitis. In some patients arthritis tends to run in families and can be genetic.
• Other factors that can contribute to developing arthritis include injuries (Acetabulum fracture or after fracture neck of femur), developmental abnormalities like dysplastic hip and Perthe’s disease
What are the treatment options available for arthritis?
• Conservative treatment does not play a significant role in management of hip arthritis, once it has set in.
• Initial treatment includes medications for pain relief, weight control and physical therapy.
• If other options don’t work to produce satisfactory response, one should consider hip replacement.
Indications for total hip or knee replacement
Total hip arthroplasty is usually indicated in secondary osteoarthritis (trauma, septic or tubercular arthritis, avascular necrosis of hip, Perthes, DDH), Total knee in primary /secondary osteoarthritis and inflammatory arthritis (rheumatoid, ankylosing arthritis, seronegative or psoriatic arthritis):
• Progressive original joint pathology despite conservative measures
• Pain and limitations of function affecting quality of life
• Rest or night pain
• Stiff hips /knee joint
• Severe unacceptable deformity.
Absolute Contraindications
Recent or current hip or distant infection, medically unfit patient.
Relative Contraindications
• Deficient or absent abductors /extensor mechanism function
• Neuropathic joint
• Progressive neurological disease
Knee Arthroscopy

COMMON ARTHROSCOPIC PROCEDURES FOR KNEE INCLUDE:
Knee arthroscopy is a surgical procedure that allows doctors to view the knee joint making a large incision (cut) through the skin and other soft tissues. Arthroscopy is used to diagnose and treat a range of knee problems.
- Removal or repair of a torn meniscus
- Reconstruction of a torn anterior cruciate ligament
- Removal of inflamed synovial tissue
- Trimming of damaged articular cartilage
- Removal of loose fragments of bone or cartilage
- Treatment of patella (kneecap)problems
- Treatment of knee sepsis (infection
At this point, a positioning device is sometimes placed on the leg to help stabilize the knee while the arthroscopic procedure takes place.
Preparing for Surgery::
- Evaluations and Tests
- Your orthopaedic surgeon may recommend that you see your primary doctor to assess your general health before your surgery
- To help plan your procedure, your orthopaedic surgeon may order preoperative tests. These may include blood tests or an electrocardiogram (EKG).
Admission Instructions:
If you are generally healthy, your knee arthroscopy will most likely be performed as an outpatient. This means you will not need to stay overnight at the Be sure to inform your orthopaedic surgeon of any medications or supplements that you take. Before your surgery, a member of the anesthesia team will talk with you. Knee arthroscopy can be performed under local, regional, or general anesthesia:
Positioning Once you are moved into the operating without room, you will be given anesthesia. To help prevent surgical site infection, the skin on your knee will be cleaned. Your leg will be wide covered with surgical draping that exposes the prepared incision site.
Procedure To begin the procedure, the surgeon will make a few small incisions, called “portals,” in your knee. A sterile solution will be used to fill the knee joint and rinse away any cloudy fluid. This helps your orthopaedic surgeon see the structures inside your knee clearly and in detail. Then based upon the operation either cleaning or repair of meniscus, ACL ligament reconstruction is done.
Closure A soft bandage will protect your incisions while they heal. Most knee arthroscopy procedures last less than an hour. The length of the surgery will depend upon the findings and the treatment necessary .
Dressing Care You will leave the hospital with a dressing covering your knee. Keep your incisions clean and dry. Your surgeon will tell you when you can shower or bathe, and when you should change the dressing.
Complications:
The complication rate after arthroscopic surgery is very low. If complications occur, they are usually minor and are treated easily.
Possible postoperative problems with knee arthroscopy include:
- Infection
- Blood clots
- Knee stiffness
- Accumulation of blood in the knee
Recovery: After surgery, you will be moved to the recovery room and should be able to go home within 1 or 2 hours. Be sure to have someone with you to drive you home and check on you that first evening.
Pain Management After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Bearing Weight Most patients need crutches or other assistance after arthroscopic surgery.
Rehabilitation Exercise: You should exercise your knee regularly for several weeks after surgery. This will restore motion and strengthen the muscles of your leg and knee. Working with a physical therapist can help you achieve your best recovery. Therapeutic exercise will play an important role in how well you recover. A formal physical therapy program may improve your result.
Driving Your doctor will discuss with you when you may drive. Typically, patients can drive from 1 to 3 weeks after the procedure.
Follow up After discharge, further wound care will be provided by your surgeon, who will also remove the sutures 10 to 12 days after the procedure. Follow-up examinations by the surgeon take place at 2 and 6 weeks. Further follow-up appointments with the surgeon may be arranged individually, depending on the problem in the joint and the repair that was made.

What is Low Back or Neck Pain?
Low back pain is when you feel soreness or discomfort in your lower back, buttocks, or hips. In neck pain, you have discomfort or soreness in the back/sides of the neck or upper back.
What are the causes of neck or back pain?
Usually, it’s multifactorial like lack of exercise, over activity, long sitting hours, obesity, diet & back deformity.
What are the common signs and symptoms of neck and back pain?
Pain and stiffness of the neck or back affect routine daily activities. Neck or back disc might present with numbness, burning, pins and needles, weakness in the limbs, and loss of bowel or bladder in low rear disc (sciatica) problem.
How can I prevent low back pain?
With physical therapy, exercising, and stretching, you can prevent low back pain. Diet control, weight reduction, correcting posture

When Should I Seek Medical Advice For Neck Or Back Pain?
- Age more than 50 years
- Recent history of an injury, like a fall or car crash
- Sleep disturbance
- Weight loss, fever, chills, or a history of cancer
- The trouble with urinating or controlling your bowels or weakness of limbs
Spinal injections are used in two ways:
- Diagnostic purposes: identify the source of neck or/and back problems.
- Therapeutic purposes: a treatment to relieve neck or back pain.
Most spinal injections are performed as part of a more comprehensive treatment program. Simultaneous treatment nearly always includes an exercise program to improve or maintain spinal mobility (stretching exercises) and stability (strengthening exercises).
Epidural injections
Epidural injections treat pain that starts in the spine and radiates to the arm or leg, which often occurs when a nerve is inflamed or compressed (“pinched nerve”). Epidural injections involve injecting an anesthetic and an anti-inflammatory medication near the affected nerve. This reduces the inflammation and lessens or resolves the pain.
Facet joint injections:
Facet joint injections can be done for diagnostic and therapeutic purposes. These injections are often used to treat degenerative/arthritic conditions. They are used to treat neck or back pain. These problems can cause pain to radiate into the shoulders, buttocks, or upper legs.
